 Dude note: The holidays are all about giving. So I thought I’d take the 14 days after Thanksgiving and answer 14 emails I’ve received from my fellow celiacs asking for guidance. And I’d like this to be a communal effort. My advice, shocking as this may be to hear (sarcasm), may not always be the best advice. So please chime in and lend your voice. Maybe I can clear my inbox at some point in 2016.
Dude note: The holidays are all about giving. So I thought I’d take the 14 days after Thanksgiving and answer 14 emails I’ve received from my fellow celiacs asking for guidance. And I’d like this to be a communal effort. My advice, shocking as this may be to hear (sarcasm), may not always be the best advice. So please chime in and lend your voice. Maybe I can clear my inbox at some point in 2016.
Day 6 of 14
A lot on my plate today, so let’s just jump right into today’s email.
I am a newly diagnosed celiac. I’m sure you hear from a lot of us. 🙂 I’ve had a few months to research, network, and try to navigate the gluten free life before my endoscopy. And, I know, I wasn’t supposed to go gluten free until after the biopsy, but I also couldn’t wait 3 months to feel some sort of reprieve. So I detoxed, then re-toxed for 4 weeks, got my biopsy confirmation and am now going through detox round 2. It’s not been fun, but I’ve certainly learned a lot about this gluten beast and what it’s done to me. I am my own lab rat and my own scientist.
With a long history of immunosuppressive ailments, I’ve not had great luck with doctors being able to able to troubleshoot the problems or provide me with any sort of healing guidance. I rely on them for the hard evidence stuff when we know what to look for.
My question to you is, do you find the informational follow up visit with the Gastro Doc to be helpful after initial diagnosis? Or have you heard that others have found it helpful? The gastroenterology center where I had my initial consult and procedure just sort of spit me out and noted on my biopsy result paperwork that I should schedule a follow up visit to go over the diagnosis. Yet they can’t get me in until December. That’s a long wait and I will be well into traversing a gluten free, gut healing existence. So I’m not really seeing the point.
I guess I’m wondering what you and others have experienced.
Thanks! Your blog is a helluva find 🙂
Great question (and I now realize I need to start using the word “helluva” more often in my blog. I love that word!)
I’ve received so many doctor horror stories when it comes to celiac disease over the years, I can see where your doubt comes from. It’s frustratingly well-founded.
Even though my doc was great and did an amazing job diagnosing me right off the bat, there was no follow-up care initiated on his end. After a year or two of not healing, I went back to him a few more times thinking something else had to be going on. But nope…it just took my body a few years to heal. I even got a second endoscopy. All was good.
But honestly…there is only one thing for you to do after the celiac diagnosis: eat 100% gluten-free for the rest of your life. So I’m not sure of the necessity of a follow up visit, unless they had a dietitian on staff who can help you with your new diet. Even then…not sure what he/she could offer.
Here’s what I would say. If you feel like you need some reassurance and you trust your doc, it can’t hurt to go back for the follow-up. But I would go in armed with questions to ask and any problems you are having. The one great thing about our disease is that it (usually) does not mean a lifetime of doctor’s visits. There is one treatment…and it is completely non-medicinal. Actually pretty cool when you think about it.
Have a helluva day everyone!



I had a follow up with my gastroenteologist after my diagnosis which was about 3 months after. Fortunately he arranged for me to see a dietician a day or so after diagnosis and they provided good information but nothing I couldn’t have found online.
His suggestion was to join a support group which I haven’t done yet but it sounds like solid advice. As I said in a previous post, nobody “gets” what it means to be Celiac except fellow Celiacs.
My GI suggested the same thing on joining a support group. Probably the best advice he gave. Your local CSA group has all sorts of information and is filled with people tackling the same challenges as you.
I was diagnosed in 2003 and met with a nutritionist. I assume she had no idea what Celiac was because she said (and this is true), “You know, going gluten free is like driving a car. You know all the rules, but it’s okay to cut corners.” Worst $200 I ever spent.
My pro tip to newbies: It takes time to feel better. It took me a whole year to feel normal again. Going GF can be really difficult and expensive (new toaster, new hot pads, more expensive food) and it’s worse when we don’t even feel better right away! So if you still aren’t 90% – 100% after 3 – 6 months of being strictly GF, then I’d consult a doctor who is not a moron about our disease (easier said than done) to see what else could be going on.
Follow up care is important, but you will likely have to guide that follow up with your research. I had a vitamin panel done and a bone density scan done. I found I had low vitamin D and osteoporosis. It was important to know that so that I could take additional steps to correct it. Also, I’ve seen my GI a handful of additional times for reassurance and follow up testing to be sure nothing else was going on. I had the same experience as GD though, nope, just takes time to heal.
Thx for the share. What did you do for your osteoporosis?
I take Vitamin D3 liquid rapid absorb vitamins. Take long walks and make sure I keep to my strict GF diet.
Don’t forget the Vitamin K2 to help absorb the Vit D3 & Calcium/magnesium!
Yep, GF and heading to grain free for me….just feel better.
I was diagnosed in April 2015. I had a three month follow up with my gastro and she didn’t even take blood or anything. All she took was my $50 copay. It was totally unnecessary.
If you feel you are staying 100% gluten free and aren’t worried about symptoms then sure, skip the follow ups. But I feel that my one year blood test (negative) and two year endoscopy (fully healed!) results gave me an enormous sense of peace of mind. It also confirmed that I’d been doing a good job staying gluten free, and that any GI distress was probably something else other than gluten. The major celiac disease orgs recommend follow up care https://celiac.org/celiac-disease/treating-celiac-disease/
Good point re: bloodtests. I will need to follow-up with my GP for that. Unfortunately during the midst of my diagnosis my family dr retired and I haven’t met my new dr yet and she doesn’t know any of my history. I should make an appointment and get some bloodwork done for a new baseline as I was very enemic before I knew I had Celiac. I wonder if anything has changed with that regard.
I love the caption! “You have celiac disease. Eat gluten free. Buh-bye!”
Awesome.
Since celiac disease is seen in family groups, and your children may need to be evaluated one day, I wanted to share my daughter’s recent experience.
My teen daughter was diagnosed 2 months ago with celiac disease. We had a consult a couple of weeks after that with a dietitian. It was helpful but we’d learned a lot on our own and some of it was repeat information. I am glad we didn’t pass up the opportunity, though. I have a friend with Celiac, and know several folks who have either a wheat allergy or are gluten intolerant. We eat with them once a month at a church potluck. And yet we were still so ignorant! My daughter was not that impressed with the dietitian since my daughter is a smart girl and she knows how to use the internet. But she agreed with me that we did learn at least one critical piece of information from her. We learned about malt (from barley, so…gluten) being in Rice Krispies. A friend with Celiac has been making Rice Krispie treats with the brand of Rice Krispies that Aldi sells (Crisp Rice, same ingredients as Rice Krispies) for her and her family, and my daughter had eaten them. We assumed since she’d been at this for a few years, and she knew more than us what was safe, but she had missed that somehow. Her children, some of whom are gluten intolerant (all teens) didn’t show any reaction to it, evidently.
The dietitian appointment was also a good time for my husband to be a part of learning about eating gluten free. If you have a significant other, or family member(s) who can go with you, I would recommend that. It’s a great opportunity for them to hear this from someone besides you, and be able to ask questions! I am the one doing all the cooking, so even though I have not been diagnosed, I would not have missed this appointment. If you have kids in school, they will help you figure that out, too. (We homeschool, so not so much of an issue for us there.)
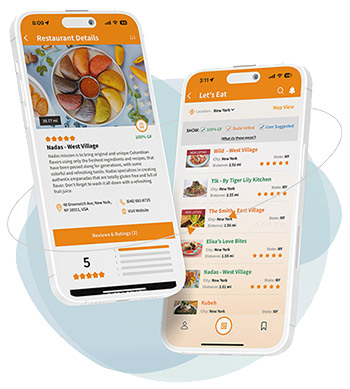
I asked the nurse there if she could recommend a restaurant nearby where we could eat lunch after the consultation with the dietitian. This worked out better than where we ate after our second doctor visit (before diagnosis) — Panera Bread! Her recommendation was a good experience for us, as the restaurant caters to diners with food allergies. Everything gluten free is served on a red plate. If there’s a gluten free diner at your table, there’s a discreet red card placed on your table so that all wait staff is aware. I’m so glad the nurse suggested it! The doctor’s office is not in our town, and I would have never learned about this place. It’s kind of a hidden gem.
I wonder if folks in the pediatric world are better with celiac patients? Everyone we have run into has been helpful, kind and not dismissive at all. This is good news for our children! Although my daughter has had symptoms coming on for years (looking back, I see this now whereas I didn’t before), we did not take her to a gastroenterologist until this past summer. It took weeks to diagnose her, not years. Her first visit with the pediatric gastroenterologist was August 21. Her diagnosis was September 30. It took me two weeks to get her blood work and x-rays done or it could have been quicker! They are catching onto this and children are benefiting! I am so thankful for that.
We are scheduled to have a follow up visit with the pediatric gastroenterologist in about a week. He has been such a great source of information. He is the one who scheduled bloodwork at the first doctor visit with my daughter, and suggested an endoscopy as soon as he saw the results. I fought him on it, because I didn’t think she had Celiac and an endoscopy seemed invasive. We had no idea. Bread was a “safe” food for her. (She would agree with me on this.) We we didn’t know anything! (She also has acid reflux and we blamed some things on that.) We didn’t see the pattern of symptoms related to gluten. He patiently explained why she should have the endoscopy, and reality sunk in that she probably did have celiac. A different doctor in the practice had an opening for an endoscopy the following week, and our doctor emailed us with the diagnosis one week later.
There have been some really rough patches. I emailed the doctor about some things that were going on, and he responded the next day. Even though there’s not a whole lot he can do at this point, he has affirmed that we are on the right path and it will get better. In that way, you are kind of on your own. (Here’s your diagnosis, buy-bye.) It’s not been easy and there are still symptoms. We never know for sure if she’s been glutened or if it’s just a part of the process. There are still 4-5 hour naps some days (among other things) but they are getting less frequent. I think the doctor will want to do bloodwork again in 3 to 6 months to make sure her tTg numbers are falling since eating gluten free. There could be hidden source of gluten preventing healing and we have heard that it will show up there if there is. We are still learning, (so much!) and have recently decided oats aren’t working out, even if they are certified. I won’t get into all the questions I still have!
This blog has been such an encouragement and source of information to me and my daughter. Both kinds of support have been great. Information and advice from the Celiac community (people who have been there!) is what gets us through, day by day. We’ve made contact with a local blogger who ran a support group for years, and that has been helpful, too. (My daughter isn’t interested in a support group right now.) A good working relationship with the doctor has been critical and it’s a shame all doctors aren’t as helpful. I guess once diagnosis is made, their job is done sometimes. Once my daughter’s tTg numbers show progress, we will know we are doing something right. She feels much better, but it is a process and she’s still healing. I wish it were quicker. The non-digestive symptoms have been the hardest for me to watch her go through, although those stomachaches are no laughing matter either.
I have my own digestive issues, and in the adult gastro. world, I find that they are just not so concerned sometimes and not as responsive, and I have to advocate for myself. It’s frustrating. But I do need my doctor and couldn’t do without him. I have wondered if I should move on to a different doc, but as of right now, I’m staying put.
Best of luck to you. And thanks, Gluten Dude, for sharing your life with us. You are awesome.
I personally have not found my GI doc to be much help in follow up, but my nutritionist was heaven-sent. I purposefully scheduled my appointment with her about a month after diagnosis and went in armed with all of the questions I had after striving to be completely gluten-free. She answered everything in more detail than I was expecting and had amazing resources about products, restaurants, label reading, etc. I would strongly advise starting any follow-up appointments with a “this-is-what-I-already-know” speech, to avoid the barrage of baby talk : “gluten is in things like bread and pasta… Blah…blah…eating it will make you sick…blah…blah” This pre-lecture has saved me from sitting though a lot of patronizing speeches and helped me maximize my appointment time getting real help and answers to questions.
My daughter’s gastroenterologist was also unhelpful. We were told it would take six weeks to get an appointment with a nutritionist at the hospital. We were fortunate to find a celiac specialist in our area who guided us through the first few months, and has her do annual blood panels to make sure she is not nutrient deficient. Good luck!
When My 6 yr old son (at the time) was diagnosed I was in shock and had no idea what anyone was talking about. ..(he’s now 12 and shortly after his diagnosis I found out I also have celiac) his doctor sent us to the worst possible nutritionist who we waited weeks to see, was actually researching celiac while I was in her office knew less than I did. Every thing that ever helped me understand the disease and stay safe I learned in a support group. From people who live it every day.
So it was no shock to me that when I went to the GI for myself and he took one look at my overweight 36 year old body and said you DONT have celiac, and I continued to ask for a blood test then schedule an endoscopy… my bad, with the same GI doc…. when the results came back positive he looked puzzled and just said ” eat gluten free” .. I never went back. Ever.
We have a GF house and so very rarely eat outside the house… if we get contaminated.. it sucks, but we just wait it out and remember to be extra careful. I haven’t found any follow ups for my son to be helpful at all.
My son was diagnosed at Children’s in Hartfort, CT (I mention this because they’ve been stellar and totally supportive) and his GI wants yearly visits to go over his general health, log any growth, and do a blood test. She said the blood test is crucial, because it shows better than anything else if something is wrong that requires further examination like an endoscopy. While he’s young and still growing, this makes sense of course, but she said it would be even more important as he got older and went out into the adult world, where it was far more likely that he’d be exposed and damage would occur.
So yes, follow-ups are important. Insist on a blood test, if nothing else.
I can’t say whether or not I think the initial follow-up would be important, but I will echo what other posters have said: make sure you have a good doctor providing long-term follow-up care. You should be having vitamin testing and regular testing for anemia. I do my best to have my celiac panel repeated at least every couple years, just to be sure that the antibodies are staying where they should be. Bone density scans are important too – even if you’re young – especially if it took a long time to get diagnosed.
I have not personally found seeing a dietician to be of any use to me whatsoever. They have all known less than me about the gf diet and had little interest in discussing particular challenges I was having and helping me to overcome them. That said, if you can find one who is extremely knowledgeable about the gf diet and provides real personalized care, I can see how that would be very valuable.
Doctors can definitely be frustrating when it comes to celiac disease, but when you find a really good one, they are a fantastic ally to have in your corner.
I found my GI to be the least significant person in my medical sphere post diagnosis. I followed up with my GI to check on healing and check in with him once a year to check vitamin and thyroud levels and that’s pretty much all I see of him. Generally, I find him extremely unhelpful.
I think the most helpful person was a registered dietitian after my diagnosis. She really helped walk me through different foods and we also did what she called a “recovery diet.” For about a month after diagnosis I eliminated gluten, but also dairy and other inflamatory foods to let my guy heal. With her guidance we brought foods back to make sure nothing else made me sick. She was also helpful with regards to learning to read labels and finding gluten-free alternatives. After a while I started talking with my regular doc(who I love) and we started doing a systems analysis. We sort of went through my body to make sure things were functioning again since I virtually everything was ailing before diagnosis. She referred me to the appropriate people as we found issues, such as PT for my muscles which had become extremely weak and a fertility specialist since that system really took a hit.
My son and my best friend have celiac. Both needed to have follow up blood tests after their diagnoses to see if their iron levels were back where they should be. With my girl friend recently she was feeling really run down and her doctor had her take another blood test. It turned out that not only was she still really low in iron but also B12 and folic acid. Her doctor told her that with celiacs low iron, B12 and folic acid can be a problem even after going gluten free.
Follow up with any doctor but my primary has been useless. My primary doctor listens to me, and knows that because I have been researching this disease for 16 years now, I know more than her about it. We test blood yearly for gliadin antibodies and TTG, and we test every 6 months for vitamin deficiencies and a nutritional iron panel. I was anemic, and I take lots of vitamins because I am low in so many. Fat soluble especially. Those can build up and be toxic, so they must be monitored. My initial follow up with gastro was pointless, as was the appointment with nutritionist, who knew next to nothing about eating gluten free (“just don’t eat bread or pasta”).
Hi- I’ve written a couple of comments, but none on recent posts til now… I had a scope + biopsy yesterday, and prior to it, my gastro told me my level indicating celiac disease was elevated.
It’s surprised me a little- I was expecting stomach ulcers (none, but gastritis coz I’m a dumbass and kept taking too many antiinflammatories for my joint pain)
And I wondered if there was something actually wrong with the IBS that I’ve had for 20 years…
I don’t have any known celiacs in the family so wasn’t even going there in my head.
Now I’ve spent all night up reading, I see so much of myself in the symptoms. So many years. With a seeming acceleration in symptoms the last two years.
According to my research- and I’ll properly verify this with the govt coeliac site- to be declared gluten free in oz food must have zero detectable gluten.
That we have the most stringent gluten standards in the world.
If this is true, does this mean I can use more of the ‘replacement’ foods? I’m ok with having to change my diet. A lifestyle change is long overdue.
I’ve been putting myself in the too hard basket for too long. I assumed it was the depression. Maybe it is.
I have mixed feelings about celiac- the ‘omg, it’s hard, it will totally change my life and I’m not an organised person’
And the other side- if my symptoms were just halved I’d be a happy camper. I’ve been avoiding fad diets and promises; it would be a bitter irony if my diet was the problem all along.
I’m a fortunate woman- my husband is a softie, so can’t rely on him to give me death glares if I’m being bad- but I can 100% rely on him to back me up. I think he would be thrilled if I felt well again.
I live life around it, but I’m tired of being tired.
If it’s positive, I’ll do it, and the other stuff I need to fix. If it’s negative, I’ve had inspiration here to get off my butt and sort the other stuff out.
If a sick celiac can, I can. And if I’m a sick celiac I can.
Thanks for being company this long night… Lucky I work weird shifts and today is a day off 🙂
Thank you all so much for sharing your thoughts and experiences. I certainly plan to keep tabs on things via blood tests with my GP. That’s something I’ve grown pretty accustomed to already, so what’s a few more tests thrown into the mix. 🙂 I guess I felt a little guilty dismissing the GI follow up visit, but I just didn’t have a good feeling about it based on how they handled my questions about that visit (very vague and dismissive). These were also the same folks that offered me my choice of crackers or pretzels after my endoscopy. The irony didn’t dawn on me until the propofol fog wore off.
Anyway, I am not wanting to be cynical about the docs. I appreciate them for what they do. But I am seriously struggling with the gluten withdrawl. My body is now in a constant state of histamine response, I have less energy than ever, muscles are weaker than ever, and my gut is in upheaval. None of my systems seem to know what to do in the absence of the gluten it’s been primed to fight. It’s a little devastating that I feel worse now, after almost 2 months gluten free, than I did when I was basically poisoning my body. I don’t know if this is how it’s supposed to go, and I will eventually start to feel better. Or if I’m doing something wrong, or if something else is maybe going on. So many questions, so much uncertainty.
I am committed to a gut healing diet, and will do my best to stay optimistic. Now if my gut would just get the memo and get to the healing.
Yep, Me and my gut feel each and everyone of you. I lucked out with the doc/dietician and the support group in that order on the same day….one week after diagnosis.
However, if any of you ever get the chance to lay your hands on The gluten free diet book by Shelley Case, RD AND fellow Celiac….get it! just graduated, she was one of the poorly trained dieticians counselling us and did something about it—research which eventually turned into a book. She is a FABULOUS speaker/presenter and travels the world. Diagnosed 20 years into her career……she totally understands even 10 years later. She works tirelessly to improve the GF world (products, laws, testing, books, education, etc). The woman is a force to be reckoned with….on our behalf! 🙂
It does get better……just as my fabulous GI says, listen to your body (yes, really!) and more specifically your gut— TRUST IT! Something doesn’t feel right, DO something about it! Don’t take “buh-bye” for a positive answer!
It does get better…..I am 2 years & 3 months into this journey. Better but not quite healed….it is easier to think and advocate for myself!
GF hugs to the community and welcome newbies!
Since my DX in 2013 I’ve been getting semi-annual blood tests to measure my gluten antibodies as well as vit B12 and blood iron (I was slightly anemic pre-DX which ultimately led to the DX).
But I’m always the one initiating the request for these tests. I don’t have doctors coming after me reminding me it’s time to get tested, or telling me what to get tested for. It took 18 months, i.e. not until 3rd test post-DX, of eating GF for my antibody levels to drop into the negative range where they’ve stayed ever since — still eating GF of course and NO cheating.
Wondering if there’s anything else I should be getting measured in these checkups every six months.
I also saw a nutritionist soon after my DX and she advised me to avoid consuming certain foods/nutrients together as it could hamper absorption of certain nutrients. The two main ones she mentioned was that tea should not be consumed with iron-rich foods as it inhibits iron absorption (I’d always been a tea drinker but now it’s only between meals instead of with), and that calcium-rich foods should not be consumed with iron-rich foods as they each interfere with the absorption of the other nutrient.